Reporting back from the Call to Action on Antimicrobial Resistance in Accra, Ghana
Dr Susie Sanderson
FDI speaker and president of the British Dental Association
Dr Susie Sanderson, FDI speaker and president of the British Dental Association, attended the second Call to Action on Antimicrobial Resistance (AMR) from 19–20 November in Accra, Ghana. The meeting aimed to build global consensus around priority areas, address knowledge gaps, and further collaboration across all implicated sectors to tackle AMR. The first Call to Action was held in Berlin, Germany, in October 2017.
What is antimicrobial resistance?
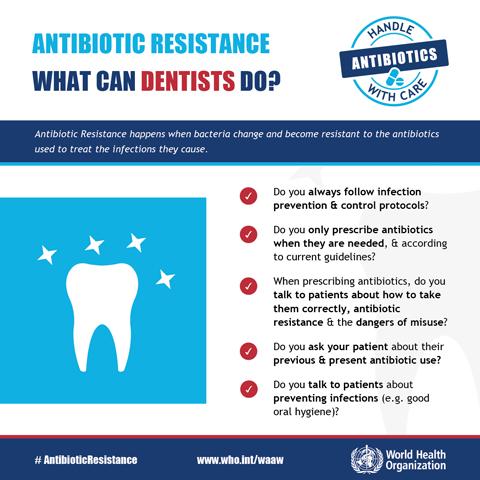
According to the World Health Organization (WHO), AMR occurs when infection-causing bacteria adapt and develop a resistance when they are exposed to antibiotics. As a result, the drugs are unable to fight the infection, which continues to harm the individual and increases the risk of spread to others. As dentists are among the most frequent prescribers of antibiotics, they are implicated in the fight against AMR, together with other health professionals. They have a responsibility to prescribe antibiotics only when they are needed and inform the patient of proper antibiotic use, associated risks, and infection prevention strategies.
Outcomes of the meeting
FDI interviewed Dr Sanderson for her take on the outcomes of this meeting as well as details on an upcoming FDI white paper on antimicrobial resistance and stewardship in dentistry.
Tell us a bit about your impressions of the meeting.
This second Call to Action on AMR welcomed 300 delegates from across the world and was sponsored by the governments of the UK, Thailand and the Republic of Ghana, as well as the Wellcome Trust, the UN Foundation and the World Bank.
Right from the start, there was an exciting and inspiring atmosphere of positivity and collaboration. It was good to see some familiar faces – and plenty of new ones. There were many opportunities to speak informally with enthusiastic and knowledgeable people not only from the wider ‘one health’ communities but also from industries and organizations that have significant contributions to make to the global efforts to reduce the level of antimicrobial resistance.
Perhaps, if I highlight some of the main facts this will help give some context to the meeting:
- If AMR is unchecked, there will be 10 million deaths in 2050. This number dwarfs the predicted deaths from cancer and road traffic accidents.
- 2 billion people do not have access to the antimicrobial they need. At the same time, the quality of medicines in some countries gives grave cause for concern. Access to antibiotics can be too easy. Some countries don’t have the regulatory capability to clamp down on unregulated sales and use.
- Surveillance of prescribing, resistance levels, and disease levels is patchy across the world and the data we do have, even when robust, is not always translated into knowledge.
How would you evaluate the overall progress achieved since the last Call to Action in Berlin?
There is no doubt that progress is being made, but there is still so much to do. My personal view is that it would be good to hear the overall narrative change from “We need to…” to “We are achieving…” Collaborations between countries and agencies are making a difference.
The Tripartite Collaboration between the WHO, Food and Agriculture Organization of the United Nations (FAO) and the World Organization for Animal Health (OIE) reinforces the ‘one health’ multisectoral approach. Alongside to advise and in consultation with the Tripartite Collaboration is the UN Interagency Coordination Group on AMR (IACG) established in 2016 and reinforced in 2018.
We heard some case studies from countries that had received funding to assist in the implementation of their National Action Plans (NAP). In Timor Leste, the NAP proposes a ‘one health’ approach with a comprehensive vision, strategy research agenda and awareness-raising campaign. The public agrees that antibiotics should be prescribed by a doctor or nurse. However, there is a persisting belief in Timor Leste that it is acceptable to use other people’s leftover antibiotics.
There are many small stewardship projects being run across the world to engage civil society. A small team from India described the ‘Superheroes against Superbugs’ intervention which has successfully helped schoolchildren understand the risks of AMR, how they can be part of the solution and how they can share the information with others.
The ability to amplify the immediate outcome of such initiatives is important to sustain the initial investment of time, money and effort.
Why is dentistry important in the fight against AMR? How does FDI plan to respond?
Dentistry is a significant player in the fight against AMR because we know that up to 10% of antibiotics in primary care settings are prescribed by dentists. We also know that a significant proportion of antibiotics in dentistry continue to be prescribed inappropriately. Dental teams also provide healthcare services for the public that include frequent surgical interventions and opportunities for inadvertent cross contamination. This means that we share the responsibility with our other human health colleagues to follow best practice procedures in Infection Prevention and Control (IPC) and to prescribe appropriately by following evidence-based guidelines. It’s both a leadership and individual challenge.
I’m very excited that the FDI Science Committee has established an AMR Working Group and is currently drafting a white paper on antibiotic resistance and stewardship in dentistry. It’ll be ready for the FDI World Dental Congress taking place from 4–8 September in San Francisco, next year. The purpose of the white paper is to describe dentistry’s significance in playing a full part in combatting the rise of antimicrobial resistance. It will also suggest ways to help dentists to engage in stewardship actions that will not only help the global situation but also directly impact the well-being of our own patients.
You may be interested in...
Ideas on antimicrobial resistance (AMR) – highlights from the Call to Action 2018